A Faith-Based Safety Plan for Diabetics Who Want to Move Without Fear
⚠️ IMPORTANT MEDICAL DISCLAIMER This content is for educational and inspirational purposes only and does not constitute medical advice, diagnosis, or treatment. Always consult your healthcare provider, endocrinologist, or certified diabetes educator before starting any exercise program or making changes to your diabetes management plan. Blood sugar targets, medication timing, and exercise recommendations vary significantly based on individual circumstances, type of diabetes, medications, complications, and overall health status. Never adjust medications or ignore symptoms without professional medical guidance. If you experience severe hypoglycemia, loss of consciousness, or any medical emergency, call 911 immediately.
🙏 “You were made to move—not fear the movement.”
📊 Did You Know?
- Over 37 million Americans have diabetes—that’s more than 1 in 10 people! (CDC, 2022)
- Regular exercise can reduce A1C levels by 0.6-0.7% in people with Type 2 diabetes
- People with diabetes are 2x more likely to have heart disease, making exercise even more crucial
- Exercise can improve insulin sensitivity for up to 72 hours after activity
When a Workout Went Wrong

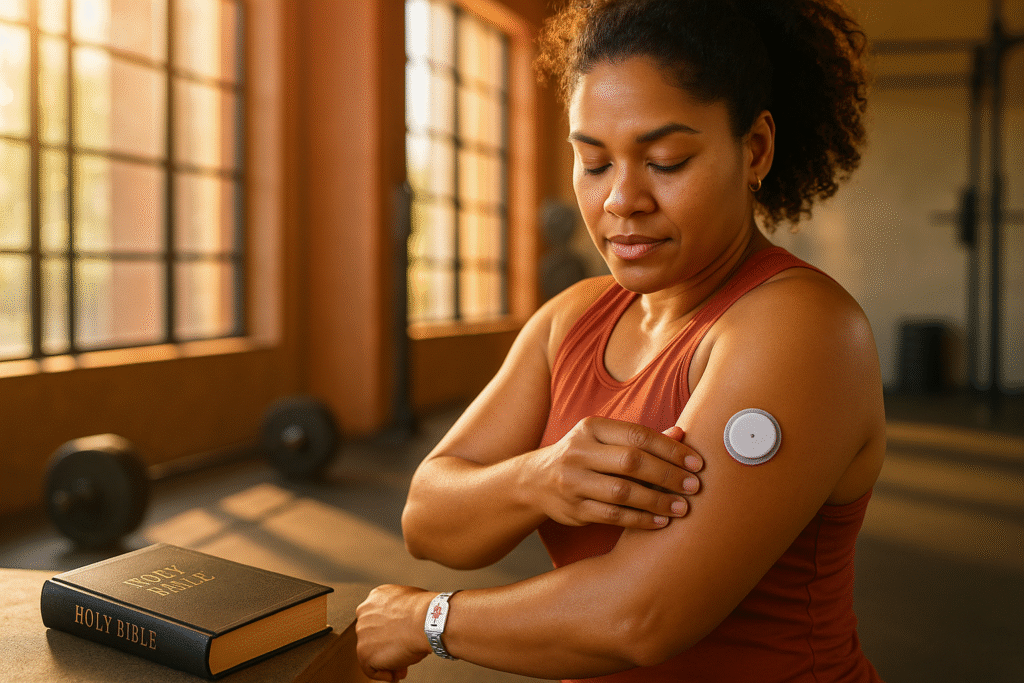
Sarah had been looking forward to her Tuesday morning Zumba class all week. As a Type 1 diabetic and faithful church member, she’d been praying for months about getting back into shape. She checked her blood sugar before class—120 mg/dL, perfect. She whispered a quick prayer, grabbed her water bottle, and headed into the studio with confidence.
Halfway through the energetic routine, something felt wrong. Her hands began to shake, but not from the music. Sweat poured down her face—more than usual. The room started spinning slightly, and she felt that familiar pit in her stomach. Her blood sugar was crashing, and she was in the middle of a crowded fitness class with no glucose tablets in sight.
💡 Diabetic Dad Joke Break: Why don’t diabetics ever win at poker? Because they always fold when their sugar gets low! 😄
That moment of fear, confusion, and helplessness is one too many of us know intimately. The shame of having to leave mid-workout, the embarrassment of explaining to others, and worst of all—the creeping dread that maybe exercise just isn’t safe for people like us.
But here’s what I want you to know: you were created to move your body in worship, not live in fear of movement. This guide will equip you with practical tips, a spiritual mindset, and a safety plan to help you exercise with confidence—but always in partnership with your healthcare team.
📖 1 Corinthians 10:31 – “So whether you eat or drink or whatever you do, do it all for the glory of God.”
Understanding Exercise-Induced Hypoglycemia
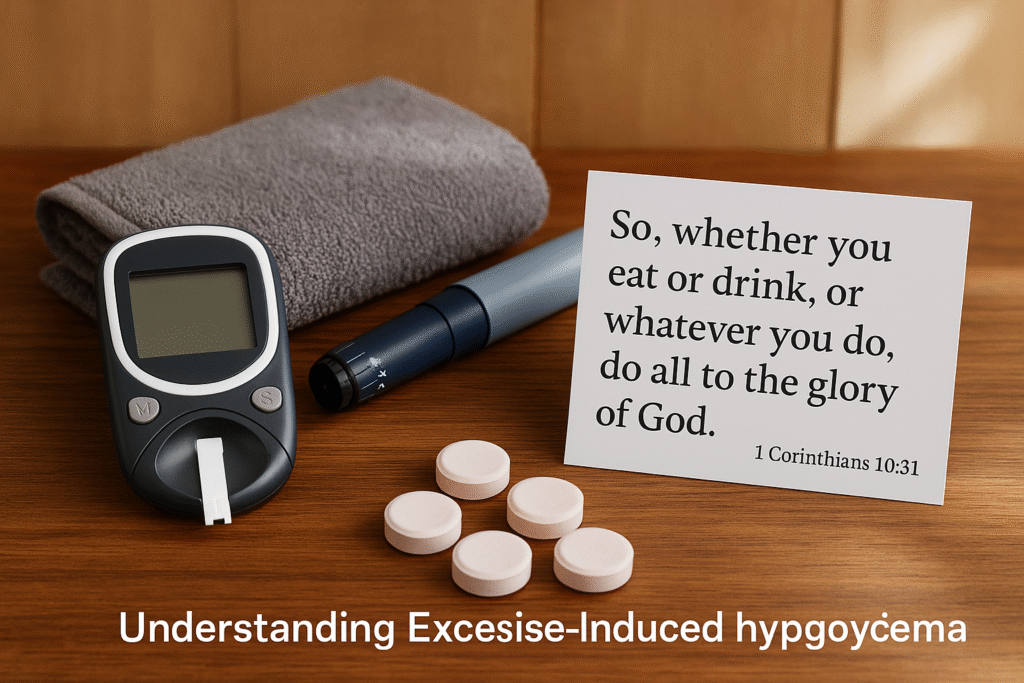
What Is Exercise-Induced Hypoglycemia?
Exercise-induced hypoglycemia occurs when your blood glucose drops below safe levels during or after physical activity. While the general definition is blood sugar under 70 mg/dL, your personal target range should always be confirmed with your healthcare provider. Some people experience symptoms at higher levels, while others may not feel symptoms until much lower.
📊 Fascinating Diabetes Facts:
- Your muscles can use glucose for energy without insulin during exercise—it’s like a secret backdoor!
- A single bout of exercise can lower blood sugar for up to 24 hours
- People with Type 1 diabetes have a 25-50% risk of exercise-induced hypoglycemia
- The risk is highest 30-60 minutes after starting exercise
Here’s why it happens: when you exercise, your muscles use glucose for energy. If you’re taking insulin or certain diabetes medications, your body may not be able to adjust quickly enough to prevent blood sugar from dropping too low. Think of it like a car running out of gas while the engine is working overtime.
The timing can be tricky. Hypoglycemia doesn’t just happen during exercise—it can strike immediately afterward or even hours later. This delayed effect is why monitoring doesn’t stop when your workout ends.
Common symptoms include:
- Sweating (more than normal for the activity)
- Shakiness or trembling
- Confusion or difficulty concentrating
- Blurry vision
- Irritability or mood changes
- Rapid heartbeat
- Hunger
- Dizziness
🤣 Another Diabetic Joke: What did the glucose meter say to the test strip? “You complete me… at least until the next reading!”
Why Different Exercises Affect Blood Sugar Differently
Not all movement affects your blood sugar the same way, and understanding these differences is crucial for safe exercise:
Aerobic exercise like walking, cycling, or swimming usually causes a steady decrease in blood sugar. Your muscles are using glucose consistently, making the effects more predictable.
Anaerobic exercise such as weightlifting or sprinting may initially raise your blood sugar due to stress hormones, then cause it to drop hours later. This delayed effect catches many people off guard.
Mixed activities like circuit training, sports, or dance classes create unpredictable blood sugar patterns because they combine both aerobic and anaerobic elements.
Duration matters significantly. The longer you exercise, the greater your risk of hypoglycemia. Sessions over 60 minutes require extra monitoring and fuel.
📊 Exercise & Blood Sugar Facts:
- Light exercise (like walking) can lower blood sugar by 20-30 mg/dL per hour
- High-intensity exercise can initially raise blood sugar by 50-100 mg/dL
- Strength training effects can last up to 16 hours post-workout
- Morning exercise typically has different effects than evening workouts due to natural hormone cycles
The Emotional and Spiritual Side of Movement with Diabetes

Acknowledging the Fear
Let’s be honest about the internal dialogue many of us face: “Will I crash again? Will others notice if I have to stop? What if I faint during the church softball game?” These fears are real, valid, and shared by countless believers managing diabetes.
📊 The Reality of Diabetes Anxiety:
- 40% of people with diabetes experience clinically significant anxiety
- Fear of hypoglycemia affects 25% of people with Type 1 diabetes
- Exercise avoidance is reported by 30% of insulin-using individuals
- Social stigma around diabetes affects 76% of people with the condition
The consequences of exercise avoidance run deeper than physical health. When we stop moving our bodies, we often experience:
- Depression and anxiety
- Guilt about poor stewardship of our health
- Disconnection from our physical selves
- Isolation from active communities
- A sense of being “broken” or “limited”
This creates what I call the shame cycle: Fear leads to avoidance, avoidance leads to guilt, and guilt feeds more fear. We start believing lies about our capabilities and worth.
😂 Levity Break: Why did the diabetic break up with their treadmill? Because it kept giving them mixed signals about their relationship!
Reframing Your Perspective
Your body isn’t your enemy—it’s God’s temple, worthy of care and movement. Diabetes doesn’t disqualify you from physical activity; it simply means you need to be more intentional about preparation and safety.
Instead of viewing diabetes management as a burden, what if we approached it as faithful stewardship? Every blood sugar check, every prepared snack, every careful decision is you caring for what God has entrusted to you.
You’re not meant to navigate this alone. God designed us for community, and that includes our health journey. The accountability, encouragement, and practical help of others isn’t just nice—it’s essential for safe exercise.
📖 2 Timothy 1:7 – “For God has not given us a spirit of fear, but of power, love, and a sound mind.”
8 Faith-Based Safety Strategies to Prevent Hypoglycemia
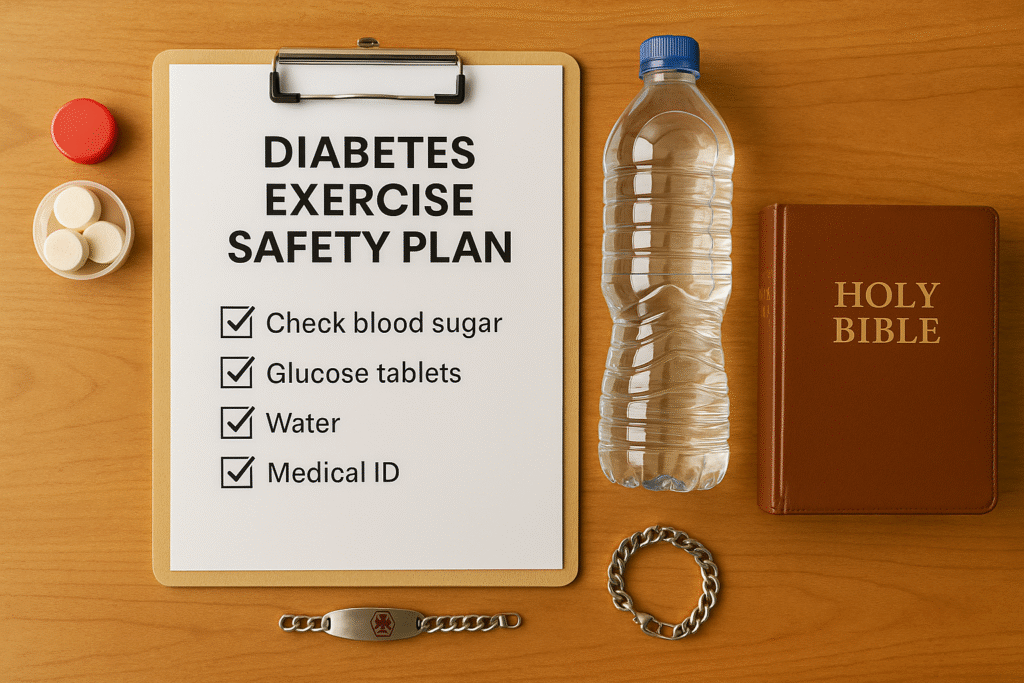
1. 🩸 Check Your Blood Sugar Pre- and Post-Workout
Before Exercise: Your pre-workout blood sugar is your safety foundation. Generally, aim for 100–180 mg/dL before starting, but confirm your personal target with your healthcare provider.
- If below 100 mg/dL: Eat 15-30g of fast-acting carbs and wait 15-30 minutes before exercising
- If above 250 mg/dL: Check for ketones and consider delaying exercise until levels normalize
- Sweet spot: 120-180 mg/dL is often ideal for most activities
After Exercise: Check within 30 minutes of finishing your workout, then again 2-4 hours later. This extended monitoring catches delayed hypoglycemia, especially after strength training.
📊 Blood Sugar & Exercise Facts:
- Exercise can lower blood sugar for up to 24 hours afterward
- People with Type 1 diabetes may see blood sugar drop 30-50% during aerobic exercise
- Stress hormones during high-intensity exercise can raise blood sugar by 40-60 mg/dL initially
- The “dawn phenomenon” affects morning exercise differently than afternoon workouts
Pro tip: Keep a simple log of your blood sugar before, during (if needed), and after different types of exercise. Over time, you’ll recognize your personal patterns.
2. 🍎 Fuel Your Body with Smart Pre-Workout Nutrition
Timing is everything. Eat your pre-workout snack 30-60 minutes before exercise to allow for proper digestion and blood sugar stabilization.
The ideal combination includes 15-30g of carbohydrates plus some protein:
- Apple slices with peanut butter
- Greek yogurt with berries
- Whole grain toast with almond butter
- Banana with a small handful of nuts
- Homemade energy balls (oats, dates, nuts)
Avoid high-fat foods close to workout time, as they slow digestion and can interfere with blood sugar management.
📊 Nutrition Facts for Diabetics:
- The average adult with diabetes needs 45-60g of carbs per meal
- Protein helps stabilize blood sugar and reduces post-meal spikes
- Fiber slows carb absorption—aim for 25-35g daily
- Timing of meals affects insulin sensitivity by up to 25%
Scripture connection: As you prepare your body’s fuel, remember Ecclesiastes 3:1 – “To every thing there is a season, and a time to every purpose under heaven.” Taking time to properly fuel your body is wisdom, not weakness.
😄 Snack Joke: What’s a diabetic’s favorite type of music? Anything with a good beet… I mean beat!
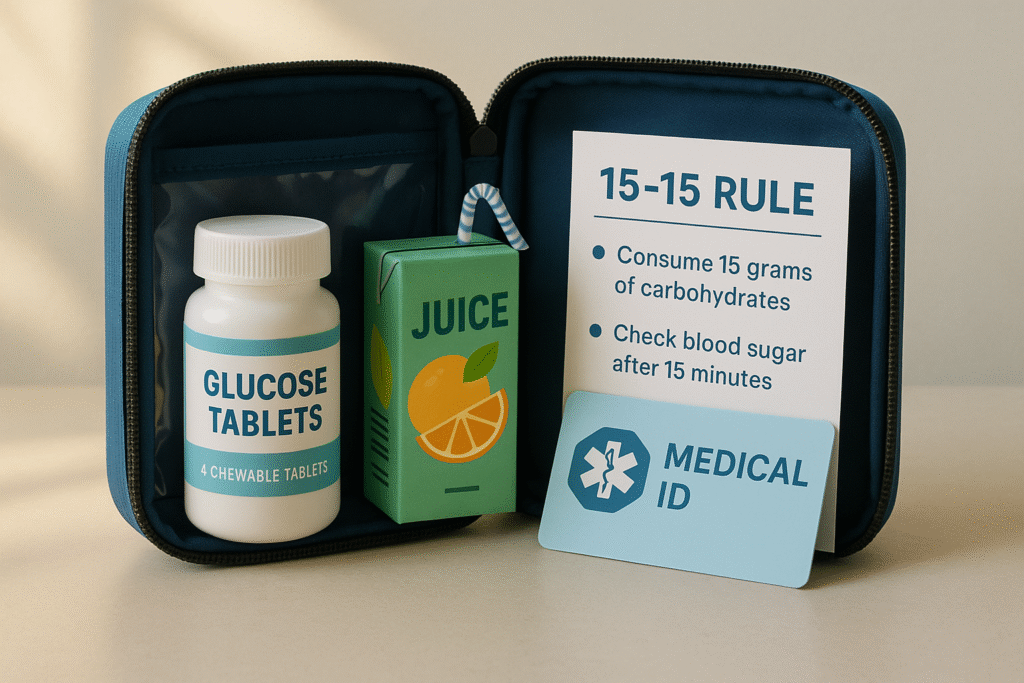
3. 🆘 Pack Emergency Glucose Every Single Time
Never exercise without fast-acting glucose. This isn’t optional—it’s essential safety equipment.
Best options for quick treatment:
- Glucose tablets (15g per dose)
- Small juice box (apple or orange)
- Regular soda (not diet)
- Honey packets
- Hard candy (like Skittles)
📊 Hypoglycemia Treatment Facts:
- Glucose tablets work fastest—raising blood sugar in 10-15 minutes
- Fruit juice takes 15-20 minutes to take effect
- Fat slows glucose absorption, so avoid chocolate for emergency treatment
- 15g of glucose typically raises blood sugar by 45-60 mg/dL
Where to keep it:
- Gym bag or purse
- Car glove compartment
- Workout clothes pocket
- Water bottle holder
Tell your workout partner where you keep your emergency supplies and how to help if you become confused or unable to treat yourself.
4. 🏥 Wear Medical Alert Identification
Options include:
- Medical alert bracelet or necklace
- Shoe tag or armband
- Smartphone medical ID feature
- Temporary tattoos for events
Essential information to include:
- “Type 1 Diabetes” or “Type 2 Diabetes”
- Emergency contact information
- Key medications
- Healthcare provider contact
📊 Emergency Response Facts:
- 73% of emergency responders look for medical alert jewelry first
- Medical ID can reduce emergency room time by an average of 2.5 hours
- 95% of first responders check smartphones for medical ID information
- Proper medical identification can prevent dangerous medication interactions
Why it matters: In an emergency, first responders can provide appropriate treatment immediately instead of wasting precious time trying to figure out what’s wrong.
🤣 Medical ID Humor: My medical alert bracelet is like my gym membership—I should probably use it more, but at least I have it!
5. 👥 Exercise with Accountability and Community
The buddy system isn’t just for kids. Having a workout partner provides:
- Safety monitoring and emergency help
- Encouragement and motivation
- Accountability for showing up
- Shared joy in movement
If you must exercise alone:
- Tell someone your plan, location, and expected return time
- Share your location via smartphone with trusted contacts
- Exercise in populated areas when possible
- Consider wearing a fitness tracker with emergency contacts
📊 Community & Health Facts:
- People who exercise with others are 95% more likely to stick with their routine
- Social support can improve diabetes management by up to 30%
- Group exercise reduces perceived exertion by 15%
- Having an accountability partner increases success rates by 65%
Church fitness groups offer the perfect combination of fellowship, accountability, and shared values. Consider starting a “Faithful Fitness” group at your church if one doesn’t exist.
6. ⏰ Time Your Workouts Strategically
Never exercise fasted. Your body needs fuel to function safely, and exercising on an empty stomach significantly increases hypoglycemia risk.
Consider your medication timing: Know when your insulin or diabetes medications are most active, as this affects your blood sugar response to exercise.
Be cautious with late-night workouts. It’s harder to recognize hypoglycemia symptoms when you’re tired, and you risk dangerous overnight blood sugar drops.
📊 Timing & Diabetes Facts:
- Dawn phenomenon causes 75% of people with diabetes to have higher morning blood sugars
- Insulin sensitivity is typically highest in the afternoon
- Late-night exercise can cause blood sugar to drop for up to 16 hours
- Cortisol levels affect blood sugar response throughout the day
Post-meal timing: Generally, 1-3 hours after eating provides the most stable blood sugar for exercise, but this varies by individual.
😂 Timing Joke: Why don’t diabetics like morning workouts? Because their blood sugar is still waking up too!
7. 💊 Understand Your Medications and Exercise
For insulin users: You may need to adjust your dosing on workout days, but never make changes without consulting your healthcare provider first. Some people reduce their rapid-acting insulin before exercise, while others adjust their basal rates.
Sulfonylureas (like glyburide, glipizide) increase your hypoglycemia risk during exercise because they stimulate insulin production regardless of blood sugar levels.
Metformin is generally safe with exercise, but stay well-hydrated and be aware of any digestive sensitivities.
SGLT2 inhibitors can increase dehydration risk, so extra fluid intake is important.
📊 Medication & Exercise Facts:
- 40% of people taking sulfonylureas experience exercise-induced hypoglycemia
- Insulin absorption increases up to 30% during exercise
- Some blood pressure medications can mask hypoglycemia symptoms
- CGM (Continuous Glucose Monitor) users report 60% fewer severe low blood sugar episodes
Always carry a current medication list and never adjust doses without medical supervision.
8. 🙏 Begin with Prayer and Preparation
Transform your pre-workout routine into worship. Instead of rushing to the gym, take a moment to:
- Thank God for your body’s ability to move
- Ask for safety, strength, and wisdom
- Surrender any fears or anxieties
- Pray for those who will exercise alongside you
Make preparation an act of faith. Checking your blood sugar, packing supplies, and planning your workout becomes faithful stewardship when done with intentionality and gratitude.
Sample pre-workout prayer: “Lord, I thank You for this body You’ve given me. Guide me as I move it in worship today. Keep me safe, give me wisdom to recognize my body’s needs, and help me find joy in movement. Let my actions bring glory to You. Amen.”
📖 Proverbs 4:26 – “Give careful thought to the paths for your feet and be steadfast in all your ways.”
😄 Prayer Humor: I told God I wanted to run a marathon. He said, “Let’s start with walking to the mailbox without your blood sugar crashing!”
Exercise-Specific Guidelines for Different Activities
Cardio/Aerobic Activities
Walking, jogging, cycling, swimming, dancing
These activities typically cause a steady, predictable decrease in blood sugar. Your muscles are consistently using glucose, making monitoring more straightforward.
📊 Cardio Facts:
- Walking for 30 minutes can lower blood sugar by 20-40 mg/dL
- Swimming engages 85% of your muscles, making blood sugar effects more pronounced
- Cycling at moderate intensity burns 300-500 calories per hour
- Dancing combines cardio with coordination, improving balance and reducing fall risk
Monitoring strategy: Check blood sugar every 30 minutes during sessions longer than one hour. For shorter sessions, pre- and post-workout checks are usually sufficient.
Fuel strategy: For sessions longer than 60 minutes, you may need 15-30g of carbs every 30-60 minutes. Sports drinks can be helpful for longer activities.
Safety tip: Start slowly and build intensity gradually. Your blood sugar response may change as your fitness improves.
Strength Training/Resistance Exercise
Weightlifting, resistance bands, bodyweight exercises
Strength training often causes blood sugar to initially rise due to stress hormones, then drop significantly 2-4 hours later. This delayed effect catches many people unprepared.
📊 Strength Training Facts:
- Muscle tissue burns glucose 24/7, even at rest
- Strength training can improve insulin sensitivity for up to 72 hours
- Building muscle mass improves glucose storage capacity
- Resistance exercise can reduce A1C by 0.3-0.5% over 6 months
Monitoring strategy: Check before exercise, immediately after, and again 2-4 hours later. Consider an additional bedtime check if you exercised in the evening.
Fuel strategy: You may not need pre-workout carbs if your blood sugar is in a good range, but be prepared for post-workout effects.
Safety tip: Don’t let initial blood sugar rises fool you into thinking you’re safe. The delayed drop is often more significant than during cardio.
🤣 Lifting Joke: Why did the diabetic’s blood sugar go to the gym? Because it heard there were going to be some serious ups and downs!
High-Intensity/Mixed Activities
HIIT, sports, circuit training, group fitness classes
These activities create the most unpredictable blood sugar patterns because they combine aerobic and anaerobic elements with varying intensities.
📊 High-Intensity Facts:
- HIIT can burn 25-30% more calories than steady-state cardio
- Interval training improves insulin sensitivity more than continuous exercise
- Team sports involve unpredictable bursts of activity
- High-intensity exercise produces more stress hormones, affecting blood sugar
Monitoring strategy: More frequent checks are essential. Consider checking during longer sessions if you feel symptoms.
Fuel strategy: Start with slightly higher blood sugar (closer to 150-180 mg/dL) and keep extra emergency supplies handy.
Safety tip: These activities are the most likely to cause unexpected blood sugar swings. Start conservatively and learn your patterns.
Group Fitness Classes

Special considerations:
- Inform the instructor about your diabetes and where you keep emergency supplies
- Position yourself near the door for easy access to supplies and exits
- Don’t feel embarrassed about stopping to check blood sugar or treat symptoms
- Bring a friend who knows your condition and can help if needed
📊 Group Fitness Benefits:
- 78% higher motivation compared to solo workouts
- Built-in instruction reduces injury risk
- Social connection improves mental health
- Variety prevents boredom and plateaus
What to Do If Hypoglycemia Strikes: Emergency Action Plan
Recognize the Signs Early
Mild symptoms: Sweating, hunger, shakiness, irritability, rapid heartbeat Moderate symptoms: Confusion, difficulty concentrating, blurred vision, coordination problems Severe symptoms: Loss of consciousness, seizure, inability to swallow safely
📊 Hypoglycemia Recognition Facts:
- 50% of severe hypoglycemic episodes occur without warning symptoms
- Symptoms can vary significantly between individuals
- Repeated episodes can reduce symptom awareness
- Exercise can mask early warning signs
Trust your body. If something feels wrong, stop and check. It’s better to interrupt a workout unnecessarily than to ignore a real emergency.
😅 Symptom Joke: My blood sugar and my mood have a lot in common—they both drop without warning and need immediate attention!
Immediate Response Protocol
The 15-15 Rule:
- STOP all physical activity immediately
- SIT DOWN in a safe location
- CHECK blood sugar if possible (but don’t delay treatment if you can’t)
- TREAT with 15g of fast-acting carbs
- WAIT 15 minutes and recheck blood sugar
- REPEAT treatment if still below 70 mg/dL
- FOLLOW UP with a snack containing protein and complex carbs once blood sugar normalizes
Examples of 15g fast-acting carbs:
- 4 glucose tablets
- 1/2 cup fruit juice
- 1/2 cup regular soda
- 1 tablespoon honey
- 15 small jelly beans
📊 Treatment Effectiveness:
- Glucose tablets: 10-15 minutes to take effect
- Fruit juice: 15-20 minutes
- Regular soda: 15-20 minutes
- Honey: 10-15 minutes
- Hard candy: 20-30 minutes
When to Seek Emergency Help
Call 911 immediately if:
- Loss of consciousness occurs
- Seizure activity happens
- The person cannot swallow safely
- Severe confusion or combative behavior develops
- Blood sugar remains dangerously low after multiple treatments
For your workout partners: If someone with diabetes becomes confused or unresponsive during exercise, don’t hesitate to call for help. It’s better to be safe than sorry.
📊 Emergency Statistics:
- 1 in 20 people with Type 1 diabetes will experience severe hypoglycemia annually
- Emergency glucagon is effective in 95% of severe cases when used properly
- Quick treatment prevents 90% of severe hypoglycemic episodes from becoming emergencies
- Delayed treatment increases recovery time by 300%
Recovery and Learning
After a hypoglycemic episode:
- Don’t immediately resume exercise that day
- Journal what happened: What led to it? How can you prevent it next time?
- Adjust your plan with input from your healthcare team
- Don’t let fear win: One episode doesn’t mean you should stop exercising
Each experience teaches valuable lessons about your body’s unique responses and helps you exercise more safely in the future.
Faith Over Fear: A Confidence Transformation Story

From Fear to Freedom
I remember the first time I worked out after my diabetes diagnosis. Every minute felt like a countdown to catastrophe. I checked my blood sugar obsessively, jumped at every sensation, and left the gym early more times than I finished a full workout.
But gradually, something shifted. Prayer became my pre-workout ritual. Instead of focusing on what could go wrong, I began thanking God for what my body could do. I started viewing my blood sugar checks not as reminders of my limitations, but as acts of faithful stewardship.
The mindset shift was profound: From “What if something goes wrong?” to “I’m prepared for whatever comes, and God is with me.”
📊 Fear & Faith Facts:
- 80% of people with diabetes report exercise anxiety initially
- Faith-based coping strategies improve diabetes outcomes by 23%
- Prayer and meditation can lower stress hormones that affect blood sugar
- Community support reduces diabetes distress by 40%
Community support made the difference. When I finally told my workout buddy about my diabetes, she didn’t see me as fragile—she saw me as brave. She learned to recognize my symptoms, celebrated my victories, and reminded me of my strength when fear crept in.
🤣 Confidence Joke: My confidence and my blood sugar have something in common—they’re both much better when I pay attention to them!
Practical Spirituality in Motion
My workouts became worship, not warfare. Each step on the treadmill became a prayer of gratitude. Every weight lifted was a declaration of my body’s God-given strength. Even the discipline of checking blood sugar became a moment of mindfulness and stewardship.
Movement as prayer transforms exercise from a chore into a celebration. When you’re running, you can meditate on Isaiah 40:31: “Those who hope in the Lord will renew their strength.” When you’re lifting weights, you can reflect on Philippians 4:13: “I can do all things through Christ who strengthens me.”
The stewardship mindset changes everything. Instead of resenting the extra steps diabetes requires, you begin to see them as faithful care of God’s gift to you.
Building Confidence Over Time
Start small. My first “victory” was a 20-minute walk around the neighborhood with my blood glucose meter in my pocket. No gym intimidation, no complex equipment—just me, my feet, and my faith.
Celebrate every success. Each workout completed safely deserves recognition. Each time you catch symptoms early and treat them appropriately, you’re building competence and confidence.
Learn from setbacks. The day I had to leave spin class early because of low blood sugar wasn’t a failure—it was proof that my safety systems worked. I recognized symptoms, treated appropriately, and stayed safe.
📊 Confidence Building Facts:
- Small, consistent actions build confidence 400% more effectively than sporadic intense efforts
- Celebrating small wins releases dopamine, reinforcing positive behaviors
- Self-efficacy in diabetes management improves A1C by an average of 0.8%
- Confidence in exercise safety reduces anxiety by 60%
Trust builds over time. After months of consistent, safe exercise, I realized something had shifted. I wasn’t exercising despite my diabetes—I was exercising as someone who happens to have diabetes, fully equipped to handle whatever came my way.
Post-Exercise Recovery and Ongoing Monitoring
Immediate Post-Workout (0-30 minutes)
Check your blood sugar even if you feel fine. Exercise can mask hypoglycemia symptoms, and you want to catch any drops before they become dangerous.
Hydrate intentionally. Replace fluids lost during exercise, but be mindful that excessive water intake can dilute blood sugar readings.
Consider a recovery snack if your blood sugar is trending downward or if you’ve had a particularly intense workout.
📊 Post-Exercise Facts:
- Blood sugar can continue dropping for 4-8 hours after exercise
- Dehydration can affect blood sugar readings by 10-15%
- Optimal recovery happens within 30 minutes post-exercise
- Protein after strength training improves muscle recovery and glucose uptake
Record your results. Keep a simple log of how different activities affect your blood sugar. Over time, you’ll recognize patterns that help you exercise more safely.
Extended Monitoring (2-24 hours)
The 2-4 hour check is crucial, especially after strength training or high-intensity exercise. This is when delayed hypoglycemia most commonly occurs.
Bedtime monitoring is essential if you exercised in the evening. Consider setting an alarm for a middle-of-night check after particularly intense sessions.
Next-day awareness: Some people experience delayed hypoglycemia the day after vigorous exercise. Stay alert to symptoms and check blood sugar if anything feels off.
📊 Extended Effects:
- 25% of exercise-induced hypoglycemia occurs 4-11 hours post-workout
- Night-time hypoglycemia risk increases 75% after evening exercise
- Muscle glycogen replacement takes 24-48 hours
- Exercise benefits on insulin sensitivity last 24-72 hours
😄 Monitoring Joke: My blood sugar is like a teenager—just when I think I understand it, it does something completely unexpected!
Learning and Adjusting
Pattern recognition becomes your superpower. You’ll start noticing things like: “I always need a snack after yoga class” or “Swimming in the morning requires less pre-workout fuel than evening sessions.”
Seasonal considerations matter more than you might think. Hot weather, high humidity, and altitude changes can all affect your blood sugar response to exercise.
Technology can help. Continuous glucose monitors provide real-time data that can transform your exercise safety and confidence.
📊 Technology & Diabetes:
- CGM users report 38% fewer hypoglycemic episodes
- Smartphone apps improve medication adherence by 56%
- Fitness trackers help identify blood sugar patterns
- Telemedicine consultations have increased 3,800% since 2020
Regular healthcare check-ins ensure your exercise plan evolves with your health, medications, and fitness level.
Your Complete Exercise Safety Toolkit
Pre-Workout Checklist
□ Blood sugar checked and in safe range (100-180 mg/dL typically) □ Emergency glucose supplies packed and accessible □ Medical ID worn and visible □ Workout partner informed or location shared with trusted contact □ Appropriate snack consumed if blood sugar below 120 mg/dL □ Prayer/spiritual preparation completed □ Medication timing considered and logged □ Hydration adequate (8-16 oz water 2 hours before)
During Exercise Awareness
□ Monitor for hypoglycemia symptoms every 15-20 minutes □ Check blood sugar every 30 minutes for sessions over 1 hour □ Stay hydrated (6-8 oz every 15-20 minutes) □ Don’t ignore your body’s signals—when in doubt, stop and check □ Keep emergency supplies within arm’s reach □ Adjust intensity based on how you feel, not your planned workout
Post-Exercise Protocol
□ Check blood sugar within 30 minutes of finishing □ Hydrate and refuel as needed based on blood sugar trends □ Record blood sugar response and any symptoms experienced □ Monitor for delayed effects 2-4 hours post-exercise □ Extra bedtime check if exercised within 4 hours of sleep □ Thank God for safe movement and celebrate the victory
Emergency Action Plan
If hypoglycemia occurs:
- STOP activity immediately—no “just one more rep”
- SIT in safe location away from equipment
- CHECK blood sugar if meter is immediately available
- TREAT with 15g fast-acting carbs (glucose tabs preferred)
- WAIT 15 minutes and recheck blood sugar
- REPEAT treatment if still below 70 mg/dL
- FOLLOW UP with protein/complex carb snack once normalized
Call 911 if:
- Loss of consciousness
- Seizure activity
- Inability to swallow safely
- Severe confusion or combative behavior
- Blood sugar won’t normalize after multiple treatments
🤣 Toolkit Joke: My diabetes supplies bag is like Mary Poppins’ purse—somehow I fit everything I need plus a few things I didn’t know I needed!
Inspiring Diabetes Success Stories
📊 Amazing Diabetes Athletes:
- Jay Cutler (NFL Quarterback): Played 12 NFL seasons with Type 1 diabetes
- Kris Freeman (Olympic Cross-Country Skier): 4-time Olympian with Type 1
- Charlie Kimball (IndyCar Driver): First licensed driver with diabetes in IndyCar series
- Zippora Karz (Professional Ballerina): Prima ballerina with Type 1 diabetes
💪 Everyday Heroes:
- Sarah, Type 1 for 15 years: Completed 5 marathons and started a diabetes running group
- Michael, Type 2 diagnosis at 45: Lost 80 pounds and reversed his need for medication
- Emma, diagnosed at 8: Now college soccer player and diabetes advocate
- Robert, Type 1 for 30 years: Climbed all 50 state high points
These stories remind us that diabetes is not a limitation—it’s simply additional information we use to live fully and actively!
Final Encouragement: You Were Made to Move
Your Identity in Christ
You are not defined by your diabetes. You are:
- A warrior, equipped for battle against fear and limitation
- A temple, deserving of faithful care and movement
- An overcomer, capable of all things through Christ’s strength
- A beloved child of God, created for abundant life
📊 Empowering Diabetes Facts:
- People with diabetes who exercise regularly live 13-15 years longer on average
- Regular physical activity reduces diabetes complications by 40-60%
- Exercise improves quality of life scores by an average of 25%
- Active people with diabetes report 70% higher life satisfaction
The Bigger Picture
Physical health supports your ability to serve God and others with energy and vitality. When you care for your body, you’re preparing yourself for whatever calling God has on your life.
Mental wellness improves dramatically with regular exercise. The mood-boosting effects of movement can be especially powerful for managing the emotional challenges of chronic illness.
Spiritual discipline is what transforms routine exercise into worship. Every workout becomes an opportunity to practice gratitude, surrender, and faithful stewardship.
Community impact happens when your courage inspires others. Every time you exercise safely with diabetes, you’re showing others it’s possible.

